Cancer researchers’ finding sheds light on COVID immunity
10 May 2021 11:00
Vaccination campaigns are running worldwide in an attempt to end the COVID-19 pandemic. In the ideal case, the current vaccines will ban SARS-CoV-2 completely. But what if we need new vaccines after a while, because of viral mutations? Researchers from the Netherlands Cancer Institute have identified new viral targets that can potentially help to develop new vaccines. They also contribute to a better understanding of the immune response against SARS-CoV-2.
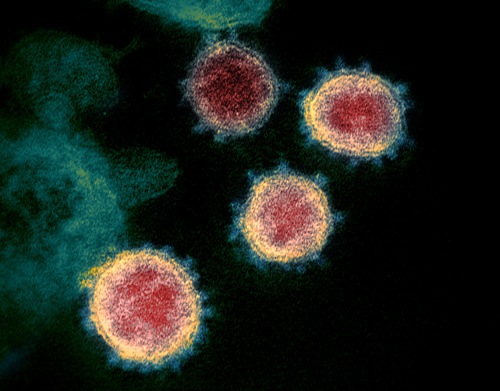
Microscopic picture of SARS-CoV-2, the virus that causes COVID-19. Image: NIAID-RML
“Last year, we temporarily stopped our cancer research and switched to studying how our immune system recognizes SARS-CoV-2”, says Anastasia Gangaev. She and fellow researcher Steven Ketelaars are excited: the results of their research have been published in Nature Communications. “Since we usually study the human immune system in relation to cancer, we already had the tools available for doing so. And now we’re finally publishing data on certain human immune cells – so-called CD8 T cells – that can recognize and kill the virus.”
Next generation vaccines
While many researchers have focused on the spike protein of SARS-CoV-2, Gangaev and her colleagues explored a broad landscape of viral protein parts that human immune cells can recognize. “Surprisingly, the most important protein part that we found is not on the spike but part of the so-called open-reading frame 1ab”, Gangaev says. “Currently all vaccines are focused on the spike protein. But, in line with other studies our data suggests that it may be important to consider other parts of the virus to elicit strong immune responses in the next generation COVID vaccines.”
Immune system memory
The viral parts that are recognized by immune cells are known by the name of epitopes. They consist of small pieces of viral proteins. “One of the epitopes we found is of particular interest, because it invokes a very strong immune response. That’s the kind of immune response you would like to elicit with a vaccine.” Interestingly, the researchers found that the immune cells recognizing this special epitope didn’t function during acute disease. “This may suggest that these specific immune cells are less likely to contribute to the damaging immune response that we’ve seen in patients with severe or critical COVID-19”, Gangaev explains. “Next to that, we saw that the cells regained their functionality after the infection and turned into a different type of T cells – so-called memory T cells – which are likely to provide at least some level of protection against reinfection with the virus”, she adds. “We’ve done tests for up to five months and the memory T cells were still there, meaning that at that time there is still active protection against the virus.”
Waiting scientists
Although most medical journals have been speeding up their publication process for COVID-19-related research, it took quite a while to publish these results. “It was a very long story indeed”, Gangaev admits. “Of course, it’s not uncommon for scientists to have to wait. We first submitted our paper to Nature around June last year. After a first revision, our publication was unfortunately rejected. At the same time we just kept expanding our research, adding new patient and sequencing data. We then redirected our attention to different journals and decided to submit our findings to Nature Communications. By the time the editors responded, we could readily answer all their questions. In the end, I think it has been a good thing our paper was rejected back in June, although we were of course very sad at the time. But in retrospect I think our publication is much more powerful now.”
Gangaev is really proud of the incredible team effort, she emphasizes. “Without that and the joined effort with the group of the late Huib Ovaa from LUMC and with Andrea Cossarizza from the University of Modena, we could never have conducted this study in such a short amount of time.”
Cancer and COVID
And now, back to cancer research? “Actually, I’m trying to do both”, Gangaev answers. “COVID-19 research has taken a lot of time last year and it was great to dive into this subject, but I definitely want to finish my other research projects as well. In addition to that, I’m going to participate in the VOICE study in which we compare the immune response of cancer patients and healthy persons after vaccination for SARS-CoV-2. This is a great collaborative effort of many different research groups and I’m glad to participate.”
Check out last year’s blog to learn more about this project and how it started
 nl
nl
 Nederlands
Nederlands