‘The Wings of Science’ – a story of basic research with real life impact
5 Feb 2021 11:05
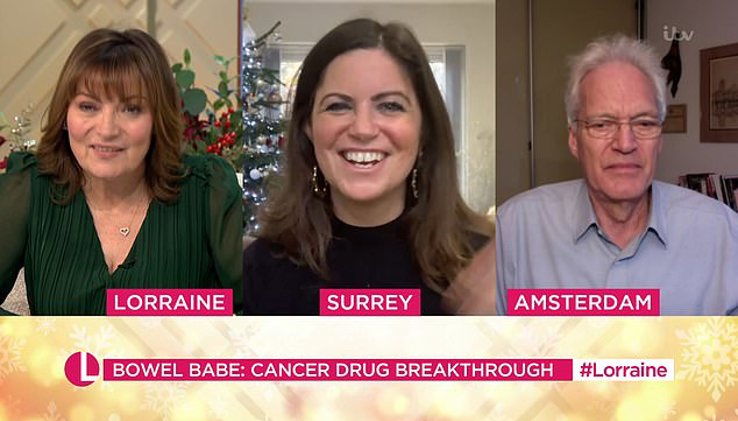
What do Dutch researcher and Oncode Investigator Rene Bernards (NKI) and British columnist and podcaster Deborah James have in common? They are both on a mission to fight cancer. Bernards’ ultimate goal is to bring his research findings to the clinic and by that to impact people’s lives. James turned her own stage 4 bowel cancer diagnosis into a mission not only to fight the illness but also to change the conversation around it. The two met in 2018: as James was running out of treatment options, it was Bernards’ innovative therapy that came to her rescue. (text by Oncode)
The team got a clear understanding of why, mechanistically, the combination became highly effective. ‘It is a novel process called synthetic lethality. It means that two events that individually are nonlethal become lethal in combination. Two drugs that don’t kill suddenly become lethal in a cocktail.’
The team proved its efficiency in animals and then together with clinicians went out to speak to pharmaceutical companies to convince them to do a clinical proof of concept study, eventually leading to the BEACON trial. It was this trial that saved Deborah James’ life.
James found out in December 2016, at the age of 35, that she had stage 4 colorectal cancer. But not the usual type - she has this rare BRAF mutation found in only 10% of the cases. The mutation makes it an aggressive form of cancer, the one that is most difficult to treat. This type of cancer gets used to treatments quickly, it is unresponsive to chemo, leaving few options.
 nl
nl
 Nederlands
Nederlands