Cellular immunotherapy with immune cells
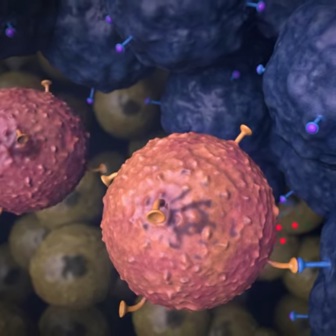
T cells are immune cells that are able to recognize foreign structures (proteins) on, for example, virus-infected cells. Through the same mechanism, T cells can also recognize abnormal proteins on the surface of cancer cells. T cells, whether or not equipped with new recognition structures, can be used as a 'living drug' for the treatment of cancer.
Cellular immunotherapy with immune cells is currently only offered in a study context for a very limited group of patients. A lot of research is still needed to make cell therapy possible for multiple patient groups with different forms of cancer in the future.
What is cellular immunotherapy?
In cellular immunotherapy, immune cells (T cells) are multiplied and/or strengthened outside the body so that they are better able to recognize tumor cells and fight the disease. These laboratory-processed immune cells are then administered to the patient via the blood as a 'living medicine'. In most cases, a single administration is sufficient.
In most forms of cell therapy, the immune cells come from the patient himself (autologous T cells), but it is also being investigated whether cells from a healthy donor (allogeneic T cells) can be used for specific forms of cell therapy.
The Netherlands Cancer Institute works with three forms of cellular therapy:
How does it work?
1. Obtaining the immune cells
In these forms of cell therapy, immune cells (T cells) are used as a 'living medicine' for the treatment of cancer. In most cases, these T cells originate from the patient himself (autologous T cells), but some forms of cell therapy use T cells from a healthy donor (allogeneic T cells).
Depending on the type of cell therapy, the T cells are obtained from the blood (via an apheresis procedure) or from tumor tissue, whereby one of the metastases of the cancer is removed through surgery. The immune cells obtained in this way form the basis of the treatment, either by multiplication alone (TIL therapy) or genetic modification (TCR and CAR T cell therapy). So a medicine is actually tailor-made for you.
From the blood; apheresis
During this procedure, the patient is connected to an apheresis device with a catheter in a vein. The apheresis device separates the required white blood cells from the rest of the blood and the machine returns the rest of the blood (including the red blood cells) directly to the patient. This process is called apheresis.
The collected white blood cells are taken to a specialized laboratory, where the T cells are processed and grown so that they can be used as medicine.
From tumor tissue
In TIL therapy, large numbers of the patient's own immune cells are returned. These immune cells originate from a tumor of the patient. Often a tumor is surgically removed for this purpose. The tumor tissue contains T cells, also called lymphocytes, that are able to infiltrate the tumor. This is why these T cells are called tumor infiltrating lymphocytes (TILs). In the laboratory, the limited number of T cells that were in the tumor is grown into eventually 'an army' of billions of immune cells.
2. Further strengthen the immune cells
For some forms of cell therapy (TCR and CAR T cell therapy), the T cells are not only multiplied outside the body, but are then further strengthened by equipping them with a new recognition structure through genetic changes that make them better able to recognize changes on the surface of cancer cells.
3. Chemotherapy
In the first week of admission, the patient receives a pre-treatment with chemotherapy that is intended to 'make room in the blood' for the edited cells.
4. Cell infusion
After the chemotherapy pre-treatment, the patient is administered the processed or multiplied immune cells. This is the actual cell therapy. Because the patient is very vulnerable during this time, this group of patients is cared for in special, sterile rooms. Visits are only allowed to a limited extent, even outside the corona pandemic.
Most patients experience fatigue and a feeling of general malaise. On the one hand because of the recovery from the chemotherapy, on the other hand because side effects of the therapy can occur. The treatment also requires a lot psychologically.
After the therapy, the patient is intensively and closely observed and mapped out how things are going, both physically, mentally, and in terms of functioning in general.
During the entire process, the patient is guided by an extensive team of medical professionals.

Cell therapy studies
In which tumor types?
The TIL therapy for patients with advanced/metastatic melanoma is the only regular cellular immuntherapy treatment.
Within a study context, patients with various forms of cancer are currently being treated with a form of cellular immunotherapy:
- TIL therapy with non-small cell lung carcinoma treated with TIL therapy.
- TCR T cell therapy and CAR T cell therapy are currently used for patients with sarcoma, lung carcinoma, renal cell carcinoma, colon cancer, testicular and ovarian carcinoma, among others.
In joint consultation between medical specialists and other practitioners, it is determined whether someone is eligible for one of the cell therapy studies.

TIL therapy for melanoma
Since 2024, TIL therapy has been one of the regular treatment methods for patients with an advanced/metastatic form of skin cancer (melanoma)
 nl
nl