Cellular immune therapy with immune cells
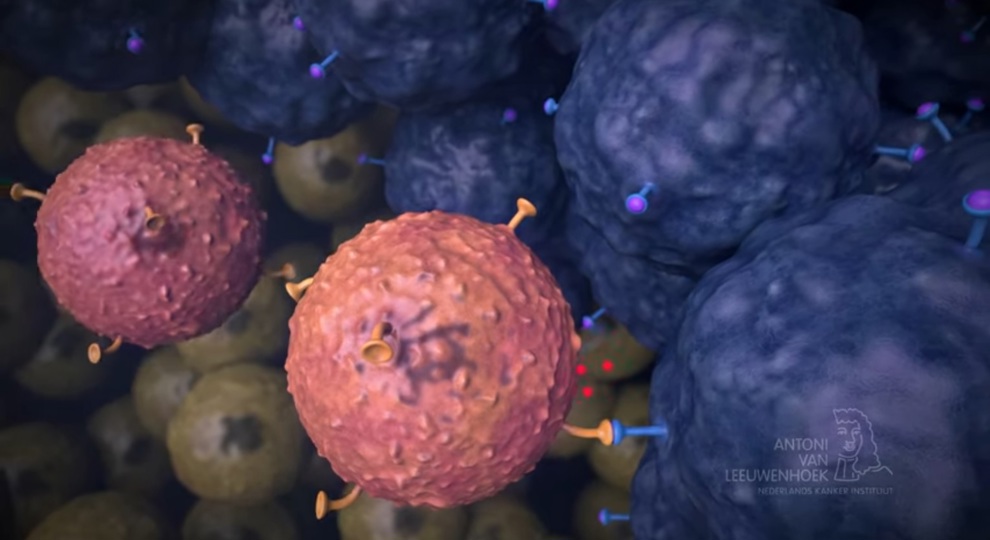
T cells are immune cells that are able to recognize foreign structures (proteins) on cells that have been infected by, for example, a virus. This same mechanism allows T cells to recognize abnormal proteins on the surface of cancer cells. T cells, potentially equipped with new recognition structures, can be used as a 'living drug' to treat cancer.
Cellular immune therapy with immune cells is currently only available as part of a trial for a very limited patient group. More research is required before cell therapy can be an option for more patient groups with various cancer types.
What is cellular therapy?
In cellular therapy, the immune cells are multiplied or reinforced outside the body so that they will better be able to recognize and fight the cancer cells. Once the immune cells have been strengthened and multiplied in the lab, they will be re-administered to the patient's bloodstream where they will be a 'living treatment'. Most people will only need to have this procedure done once.
In most kinds of cellular therapy, these immune cells are the patient's own cells (autologous immune cells), but we are looking into the use of cells from healthy donors (allogeneic immune cells) in specific types of cell therapy.
The Netherlands Cancer Institute offers three types of cellular therapy:
How does it work?
1.Obtaining the immune cells
Cell therapy involves the use of immune cells (T cells) as a "living drug" to treat cancer. Usually, these T cells are from the patient themselves (autologous T cells), but some forms of cell therapy use T cells obtained from a healthy donor (allogeneic T cells).
Depending on the type of cell therapy, T cells are taken from the blood (apheresis procedure) or tumor tissue, after the surgical removal of one of the metastases. The immune cells that have been obtained, will form the basis of the treatment, either by multiplication alone (TIL therapy) or genetic modification (TCR and CAR T cell therapy). Your drug will be made and personalized just for you.
Taken from the blood; apheresis
During the procedure, the patient is hooked up to an apheresis machine with a veinous catheter. The apheresis machine separates the necessary white blood cells from the rest of the blood, and the machine returns the rest of the blood (such as the red blood cells) directly to the patient. This process is called apheresis.
The white blood cells are collected and taken to a specialized laboratory, where the T cells are processed and reinforced so that they can be used as a drug.
From tumor tissue
In TIL therapy, large numbers of the patient's own immune cells are administered to the patient. These immune cells are taken from the patient's own tumor. This tumor will often be surgically removed to be used in this treatment. There are T cells present in the tumor, also known as lymphocytes, which are able to infiltrate the tumor. That's why these T cells are called tumor-infiltrating lymphocytes (TILs). The small number of T cells that were in the tumor are multiplied in the laboratory, where they eventually become an "army" consisting of billions of immune cells.
2. Further reinforce the immune cells
For some types of cell therapy (TCR and CAR T cell therapy), the T cells are multiplied outside the body and subsequently further enhanced by equipping them with a new recognition structure through genetic changes that makes them better able to recognize changes on the surface of the cancer cells.
3. Chemotherapy
During their first week of admission, patients receive chemotherapy as a pre-treatment, designed to "make room in the blood" for the processed cells.
4. Cell infusion
After the chemotherapy pretreatment, the patient receives the enhanced or multiplied immune cells. This is the cell therapy. Because patients are very vulnerable at this stage, the patient group will be staying in special, sterile rooms. Visits are limited, even outside of the risk of COVID-19.
Most patients experience fatigue and generally feel unwell during the treatment. This is partly due to the recovery from chemotherapy and partly due to the fact that the therapy can cause side effects. The treatment is also mentally challenging.
All patients are intensively and closely observed after the treatment. We will track how things are going, physically, mentally, and in terms of their general functioning.
Patients are supported by a comprehensive team of medical professionals throughout the entire process.

Cell therapy trials
For which tumor types?
Cell therapy is currently only available as a treatment of solid tumors only in the context of clinical trials. Patients must meet (trial) specific conditions in order to participate. In almost all cases, these patients have already undergone one or more forms of regular therapy. At the NKI, patients with various cancer types are currently being treated with cellular immunotherapy as part of a trial:
- In addition to the TIL study that's currently available to patients with advanced/metastatic melanoma, patients with non-small cell lung carcinoma are now also eligible for TIL therapy.
- TCR T cell therapy and CAR T cell therapy are currently available to patients with sarcoma, lung carcinoma, renal cell carcinoma, colon cancer, and testicular and ovarian carcinoma.
A patient's eligibility for cell therapy will be discussed in joint consultation by medical specialists and other practitioners.
 nl
nl
 Nederlands
Nederlands